Donna Burke is a mental health therapist in Dundalk, Maryland. She submitted this story to us as a guest writer.
“Is he gone?” My voice broke as I numbly asked the awkward hesitant voice on the other end of the telephone.
“Yes,” was his soft reply.
“Was he in pain?” I braced my heart for the millionth time for the typical cold, clinical response, but the cardiology fellow on the opposite end of the telephone had not yet cultivated a detached hardened tone.
“Pain,” he repeated, not certain if he heard me correctly, then warmly, compassionately, “No, no pain. He never woke up.”
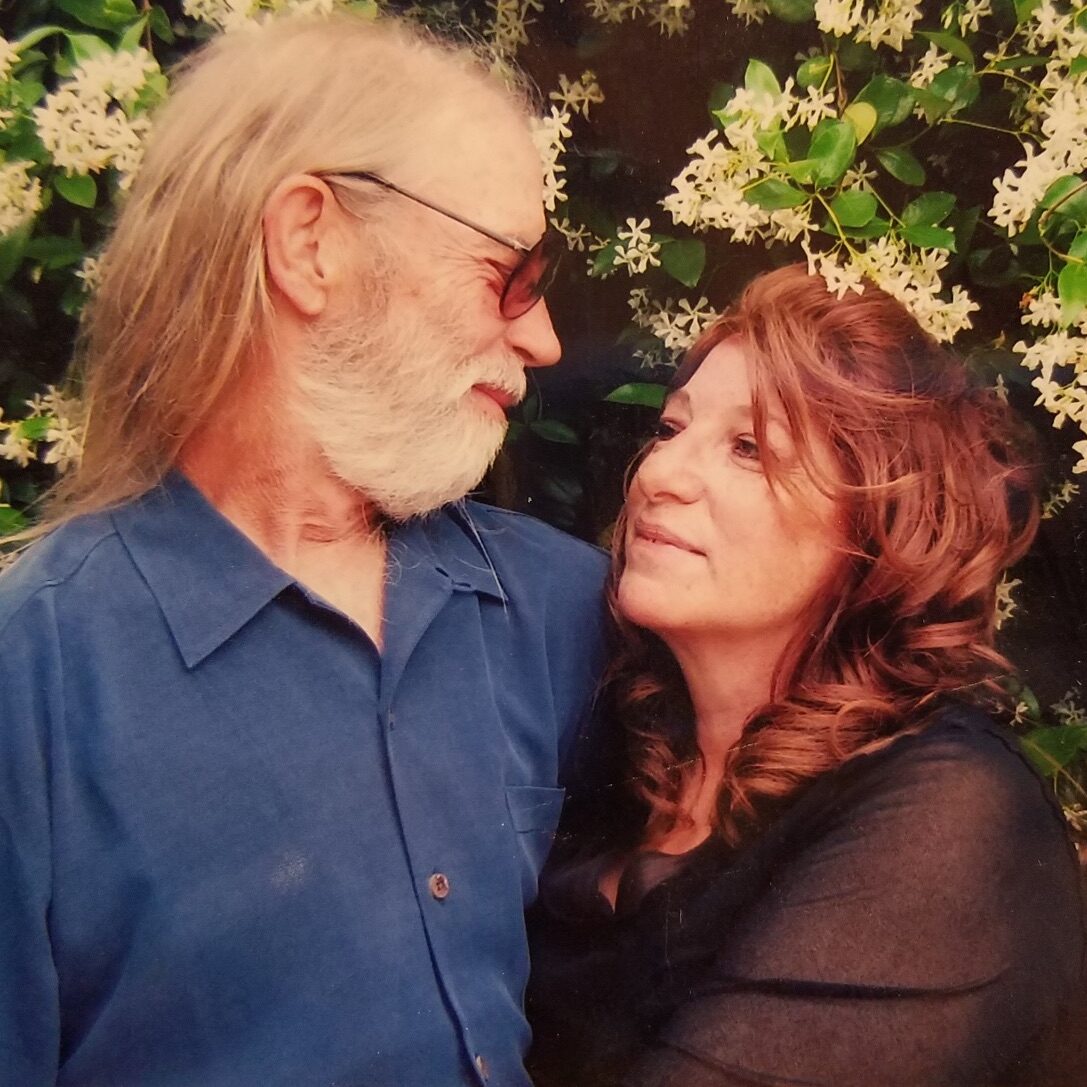
In silence, he allowed what he just told me to sink in. My beloved husband had died. I sat there in the still of that dark night clutching the telephone as I realized that I am now alone in the world. I would never hear my Eddie’s great belly laugh, or soft deep voice saying, “Good Morning, Darling,” as he came down the stairs in the morning. I wondered what I should do next. Time remained frozen.
In a fog, I realized that the doctor was still on the telephone line. Oddly, I felt sorry for him. He had the misfortune of being the cardiology fellow on call that night. He had the misfortune of being the first to respond to the Code Blue call to my husband’s room, and he had the difficult and sad task of waking his patient’s wife in the middle of the night to tell her that she was now a widow at the age of 53.

The next question that I asked the doctor is, unfortunately, not an uncommon one under the circumstances. However, I think that, perhaps, it shouldn’t be so common.
“What do I do now? I do not know what to do.”
How could it be that I spent the past four months watching my poor and frail husband’s health rapidly and seriously declining in a cardiac intensive care unit where teams of doctors fretted over him day and night, yet be completely blindsided, and in shock to receive the telephone call saying that he had died? Why was I not the least bit prepared for this?
To die with dignity is inherent in all human beings.
Death was not an end result neither Eddie’s doctors ever discussed nor I planned for. There were numerous discussions with social workers, and discharge planners about preparation for Eddie coming home, but never once was there a discussion about the very real likelihood that he could actually die.
An Expectable Death
“What do I do now? I do not know what to do,” are words of a person in shock, as if something unexpected had happened. But, was Eddie’s death really unexpected? After four long months of watching my husband’s body break down organ by organ, system by system, should his death have been such a shock?
Eddie was an insulin-dependent diabetic with very brittle uncontrollable glucose levels. He had long ago lost the sensation of feeling in both of his legs and feet due to peripheral neuropathy, which made him vulnerable for non-healing foot ulcers and chronic bone infections. Eddie had also required a kidney transplant at the age of 40, after his own kidneys had failed due to chronically high blood glucose levels. This procedure saved his life, but never really functioned as well as one’s own healthy kidneys would. Consequently, he teetered always on the verge of requiring dialysis.
Eddie had suffered four heart attacks over an eight year period before his final hospitalization in January 2014 for congestive heart failure. A proud and private man, Eddie did not want anyone to know that his conditions were as serious as they were. He was successful at maintaining an appearance of strength and health even though his coronary artery disease was so advanced that it was deemed inoperable. His heart’s ejection fraction, a number which indicates the heart’s ability to pump effectively, was about a fifth of normal, indicating a heart so weak that its pumping ability was no longer strong enough to keep up with the demands of his body.

For four months, various intensive care team doctors attempted to manage the volume overload of fluid in Eddie’s body. Each new treatment approach failed until eventually, three weeks before his death, the extreme efforts to intravenously diurese Eddie destroyed his transplanted kidney requiring him to go on permanent dialysis. Lastly, his latest foot ulcer had ruptured and was showing signs of infection. The consensus was that the foot needed to be amputated.
As he was wheeled into surgery, the vascular surgeon, who knew Eddie well, stated, “I will see you walking into my clinic three months from now on your prosthesis as if nothing has happened.”
Twelve hours later, Eddie was dead. How could the doctors not have anticipated that a man whose overall health was as jeopardized as Eddie’s might very well not be able to survive such a traumatic surgery?
Death as a Failure
I believe that this is because death is viewed as a medical failure in modern western hospitals. Consequently, Eddie’s final months were spent trapped within a culture that could not, and would not listen to him. Eddie had to recover, or their medical model, all that they stood upon and believed in would be shaken. Eddie and I had become nothing more than shadows in the room as the team of doctors continued to offer hope upon hope in the form of the latest medication, or procedure. Eddie was looking sicker by the day. He could no longer hold his head up, dress or feed himself, and he shook so badly from the side effects of the dialysis that he begged to die. The doctors would only continue to offer bright, confident predictions for Eddie’s recovery, and I grabbed these false hopes like a drowning man to a life preserver. I trusted the system wholeheartedly. Eddie, however, did not.
Eddie told every doctor who examined him that he knew that he was dying, and that he wanted to be allowed to return to his favorite place on earth—his home—to die peacefully with his wife and four dachshunds by his side. He exhibited every sign and symptom of impending death listed by the National Institute of Health. He became uncharacteristically agitated, confused, detached, and disoriented. He stopped eating, and had no control of his bowels, yet, the doctors continued to insist
that he was not a candidate for hospice care, and that they expected him to show signs of improvement “soon.” Each time that a doctor emphatically stated that my husband was not dying, I breathed a sigh of relief.
It haunts me still to think that I leaned over to whisper in his ear, “Did you hear that, Darling? They said that you are not dying. You are not a candidate for hospice.”
Eddie replied, “I heard them. They are just not hearing me.”
Dying Alone
Because he had to face so many serious health conditions over the years, my husband and I talked many times about his wishes after he died. We always believed that when his time came, we would both know it, be well informed by his doctors, and would make our decisions together when he died. But as my husband’s death approached, we consulted daily with numerous physicians who rejected his many requests to be allowed home hospice, and who dismissed his feelings as “situational depression” from being hospitalized for so long.
Because of this institutional illusion of immortality, I was not by my husband’s side when he died, as we had planned. Instead, he died alone, surrounded by machines in a sterile, stark hospital room.
I spend my days now thinking how it must have felt to be Eddie during the final four months of his life. I tried so hard to be a good wife, to bring to him all of my strength to make up for the strength that he lost daily. I tried to keep hope alive, even when the very idea of hope only caused him more pain. I dutifully listened to the doctor’s instructions. I did not dare to consider death as a real possibility, while Eddie suffered in silence, trapped in a place that would only speak to him in terms of recovery and treatment. How foreign we all must have seemed to him as he drifted further away inside his diseased body all alone.
Laws That Embrace Final Wishes
That is why I believe that we must pass humane safe-guarded choice laws in all states that embrace the final wishes of the terminally ill to die on their own terms. We must hear their voices, and give them choice and control to approach their death in a manner that is meaningful to them.
My Eddie deserved this, and so now, I must be his voice advocating for the rights that should have been his: to die with the dignity that was so much a part of the man my husband was, and which, I believe, is inherent in all human beings.